| Download | Downloads | Last Modified | Owner | Rating | Version | Name | Last Modified | Rating | |
|---|---|---|---|---|---|---|---|---|---|
| Download | Downloads | Last Modified | Owner | Rating | Version | Name | Last Modified | Rating | |
| Clinical Documents | |||||||||
| Download | 304 downloads | 31-12-2019 17:28 | landmarkaesthetics.net | 1.1 | 31-12-2019 17:28 | ||||
| Download | 273 downloads | 31-12-2019 16:47 | landmarkaesthetics.net | 1.0 | 31-12-2019 16:47 | ||||
| Download | 242 downloads | 31-12-2019 16:44 | landmarkaesthetics.net | 1.0 | 31-12-2019 16:44 | ||||
| Download | 247 downloads | 31-12-2019 16:43 | landmarkaesthetics.net | 1.0 | 31-12-2019 16:43 | ||||
| Download | 328 downloads | 31-12-2019 16:40 | landmarkaesthetics.net | 1.0 | 31-12-2019 16:40 | ||||
| Download | 274 downloads | 31-12-2019 15:39 | landmarkaesthetics.net | 1.0 | 31-12-2019 15:39 | ||||
| Download | 340 downloads | 31-12-2019 15:35 | landmarkaesthetics.net | 1.0 | 31-12-2019 15:35 | ||||
| Download | 231 downloads | 31-12-2019 15:34 | landmarkaesthetics.net | 1.0 | 31-12-2019 15:34 | ||||
| Download | 253 downloads | 31-12-2019 15:33 | landmarkaesthetics.net | 1.0 | 31-12-2019 15:33 | ||||
| Download | 226 downloads | 31-12-2019 15:32 | landmarkaesthetics.net | 1.0 | 31-12-2019 15:32 | ||||
| Download | 282 downloads | 21-12-2019 7:43 | landmarkaesthetics.net | 1.0 | 21-12-2019 7:43 | ||||
| Download | 248 downloads | 05-05-2019 15:09 | landmarkaesthetics.net | 1.0 | 05-05-2019 15:09 | ||||
| Download | 276 downloads | 05-05-2019 15:08 | landmarkaesthetics.net | 1.0 | 05-05-2019 15:08 | ||||
| Download | 273 downloads | 05-05-2019 15:07 | landmarkaesthetics.net | 1.0 | 05-05-2019 15:07 | ||||
| Download | 964 downloads | 05-05-2019 15:07 | landmarkaesthetics.net | 1.0 | 05-05-2019 15:07 | ||||
| Download | 378 downloads | 05-05-2019 14:56 | landmarkaesthetics.net | 1.0 | 05-05-2019 14:56 | ||||
| Download | 286 downloads | 02-01-2018 21:17 | landmarkaesthetics.net | 1.0 | 02-01-2018 21:17 | ||||
| Download | 286 downloads | 02-01-2018 21:17 | landmarkaesthetics.net | 1.0 | 02-01-2018 21:17 | ||||
| Download | 260 downloads | 02-01-2018 21:17 | landmarkaesthetics.net | 1.0 | 02-01-2018 21:17 | ||||
| Download | 248 downloads | 02-01-2018 21:17 | landmarkaesthetics.net | 1.0 | 02-01-2018 21:17 | ||||
| Download | 452 downloads | 02-01-2018 21:17 | landmarkaesthetics.net | 1.0 | 02-01-2018 21:17 | ||||
| Download | 255 downloads | 02-01-2018 21:17 | landmarkaesthetics.net | 1.0 | 02-01-2018 21:17 | ||||
| Download | 264 downloads | 02-01-2018 21:17 | landmarkaesthetics.net | 1.0 | 02-01-2018 21:17 | ||||
| Download | 240 downloads | 02-01-2018 21:17 | landmarkaesthetics.net | 1.0 | 02-01-2018 21:17 | ||||
| Download | 377 downloads | 02-01-2018 21:17 | landmarkaesthetics.net | 1.0 | 02-01-2018 21:17 | ||||
| Download | 263 downloads | 02-01-2018 21:17 | landmarkaesthetics.net | 1.0 | 02-01-2018 21:17 | ||||
| Download | 322 downloads | 02-01-2018 21:17 | landmarkaesthetics.net | 1.0 | 02-01-2018 21:17 | ||||
| Download | 298 downloads | 02-01-2018 21:05 | landmarkaesthetics.net | 1.0 | 02-01-2018 21:05 | ||||
http://www.gatewaylasercenter.com/apothica.html
Arabica seed oil improved skin dryness and promoted the body’s natural production of collagen and elastin.6
Coffea arabica supported improvement of the appearance of wrinkles, redness, and rough texture in a clinical trial—after just 12 weeks of twice daily application.9
Chlorogenic acid helped reduce the normal redness associated with prolonged ultraviolet exposure.7
Caffeine enhanced the visibility of skin smoothness and promoted a reduction in wrinkle depth—with clinical results seen in only 4 weeks.
http://www.lifeextension.com/Vitamins-Supplements/item80151/Anti-Aging-Rejuvenating-Face-Cream
https://books.google.com/books?id=iwwo5gx8aX8C&lpg=PA73&ots=Ux-WGhcaYg&dq=AMPA%20metformin&pg=PA76#v=onepage&q=AMPA%20metformin&f=false

|
|
|
|||||
|
|
|
| Bronze | Silver | Gold | Golden Hair |
| $720/year | $1200/year | $10,000/year | $15,000/year |
| 3 Hydra or laser facial | 4 Hydra or laser facial | 4 Hydra or laser facial | 4 Hydra or laser facial |
| 3 RF tx | 4 RF treatments | 8 RF treatments | 8 RF treatments |
| 25% off reg services | 25% off reg services | 2 ablative laser services | 2 ablative laser services |
| 25% off ZO | 8 CoolSculpting cycles | 8 CoolSculpting cycles | |
| 4 Allergan fillers | 4 Allergan fillers | ||
| 2 Versa fillers | 2 Versa fillers | ||
| 100 Units Botox | 100 Units Botox | ||
| 2 PRFM | 2 PRFM | ||
| LED and infrared laser | LED and infrared laser | ||
| 10 laser hair per area | 10 laser hair per area | ||
| 3 – 30 min vein tx | 3 – 30 min vein tx | ||
| 25% off ZO | 25% off ZO | ||
| Transplant 2500 FUE |
The Ugly Truth of Cellulite
In our aesthetic culture today, the word ‘cellulite’ has come to represent a hideous fat condition of the human body where by we will do just about anything to rid it. The term was first used in the 1920s and began appearing in English language publications around the late 1960s. The earliest reference appeared in Vogue magazine, the prestigious fashion journal. Vogue introduced this new word for ‘fat’ into American society and from then on, controversy has surrounded cellulite for decades whereby medical doctors, scientists, and other professionals cannot agree if this foundation of fat really exists. Many doctors have flatly refused to acknowledge the existence of cellulite and still do despite the overwhelming scientific evidence.
Over the last several months, I have reviewed numerous studies as my sources for this educational editorial and whether you agree or disagree, my intent is to help tear down this controversy and present solid science to facilitate the right products and cellulite treatment for a successful end point result.What is this fat called Cellulite?
Cellulite has been established as a common body fat condition occurring in women (and to a lesser extent, men) that consists of inflammatory adipose material known as one of a constellation of connective tissue disorders (CTD) with still unidentified, related causes. This unsightly skin condition is generally referred to as “cottage cheese” or “orange peel” skin and is visibly detected in the abdomen, thighs, pelvic region, and arms. Given this, it is believed by many in the scientific community that the only “true” cellulite occurs in the buttocks and thighs. These regions of fat deposit still remain another debate with the medical community and will be addressed in this editorial.
Cellulite is not related to overweight body mass; it can affect both average and underweight individuals. Because of this fact, weight loss and cellulite management are two separate issues, making this unattractive superficial fat the last to be affected by exercise and diet. Although doctors recommend a health conscious pattern of eating as a cellulite antidote, the reality is this approach does not rid the ugly fat, only facilitates prevention and the formation of excess adipose tissue in the body that later can turn into inflammatory material. This approach is used as a preventative and not a cure to the condition. Diet is only one resolution of many for cellulite management.
Cellulite is a nasty, particular form of fat trapped between water located just below the dermis that builds and begins to form ugly bumps and bulges through the skin, effecting 90 percent of women. Why are women more predisposed to cellulite than men? One reason is women organize fat parallel to their skin causing a pulling-down effect making this physiological consequence primarily responsible for the bulges in the skin. In addition, hormones, predominantly Estrogen, play a central role in the formation of cellulite. Estrogen appears to initiate and aggravate this fatty substance.

Many myths and false information surround this “dreaded dimple disease” that has led to a booming and profitable cellulite industry primarily focused on the hope of the sufferer to rid the condition. However, the science points to predisposing genetic factors such as gender, race, biotype, a hormone allele determining the receptor number and sensitivity, distribution of subcutaneous fat, and predisposition to circulatory insufficiency. Although the aforementioned are not necessarily the total cause and factor of cellulite, these manifestations have been linked to their role as primary ‘aggravating sources.’ Most cellulite ‘cures,’ by which doctors and scientists agree, have been ineffective. Recent research points to the ‘real substance’ of cellulite that actually are the product of anatomy, genes, and hormones.
Very few men are affected with cellulite. Aside from the hormone connection, one reason could be based on the composition and conduct of women’s fat cells and the connective tissue that holds them in place. Simply put, a woman’s connective tissue is inflexible therefore as females gain weight the fat cells expand, bulging upward towards the surface of the skin creating the ‘orange peel/cottage cheese’ appearance. In men, the outer skin is thicker coupled with less fat on the thighs obscuring the physiological event occurring just below the surface.
The Hormone Cellulite Influence
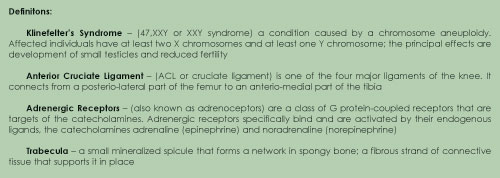
Hormones control over 300 of our body’s responses and cellulite is a target for these commandos. Although Estrogen plays a dominant and significant role, other hormones such as insulin, the catecholamine adrenaline, noradrenaline, thyroid hormones, and prolactin have all been shown to have influence in the development of cellulite.
It is common for pubescent females as young as 11 to display some degree of cellulite, thereby connecting the ‘dots’ to the hormonal component and its unwelcome ‘orange peel’ skin appearance. Cellulite is rarely seen in males but common with those men who have androgen-deficient conditions such as Klinefelter’s Syndrome, hypo-gonadism, and males receiving estrogen therapy in the event of some prostrate cancers. The cellulite becomes more severe as the androgen deficiency drops in these males, lending credibility to the estrogen hormone connection. Testosterone, the male hormone, or some modification of this hormone, is being considered as a potential therapeutic agent in estrogen driven disorders such as cellulite. Be that as it may, still little science supports the totality of comprehensive cellulite understanding and although this fatty syndrome afflicts primarily women, it also appears to bypass Asian females… leaving the question: why do some women get cellulite and others do not?
What we do know, is recent conclusive studies site that cellulite appears to occur in certain families leaving many questions to be answered. What could be the hereditary component? Is there a preventative gene, or an absent gene in the cellulite-free women? A retrospective study found genetic factors such as personal history; family history and race were the most significant predictors for the striae maturity.
One recent study, (Chang et al, 2004) asserts striae, pelvic relaxation, and varicose veins appear to be related to the action of matrix metalloproteases’ (MMP) activity initiated by estrogen and that the physical manifestations of cellulite are due to destruction of the normal architecture of collagen trabeculations that keep the adipose tissue confined to the deep and superficial fat layers. (Lockwood, 1991)
Estrogen stimulates fibroblasts in connective tissue to produce MMPs degrading the collagen fibers that make up the trabeculations in the adipose tissue. Collagenase in connective tissue destruction is partly responsible for the local spread of cancer and metastases. We know that fibroblasts in the ECM (extra cellular matrix) represent a heterogeneous population of these active cells (Sorrell and Caplan, 2004), but we know little about what controls fibroblast cell functions (Haczynski et al, 2002, Hudelist et al, 2005, Chen et al, 2003, Kokorine et al, 1997, Sorrell and Caplan, 2004).
The role of the ECM (extracellular matrix) is not fully identified in connective tissue disorders. The ECM contains structural proteins that interact with integrins on the surface of the fibroblasts, which appear capable of directing the production of either collagen or collagenase via the direction of the mechanical forces exerted on the integrins. The role of integrins in health and disease is currently a vast area for skin research.
There appears to be an inverse dose dependent relationship between the level of estradiol and the proliferation of ACL fibroblasts (anterior cruciate ligament). Fluctuation in estrogen levels have been shown to be associated with ACL injury and these disorders appear to be the result of either the direct action of estrogen on connective tissue proteins or an indirect action of estrogen mediation through fibroblasts.
Cellulite in females begins with puberty and progresses throughout their life span. After menopause, the fatty tissue stroma supplies the estrogen via conversion of adrenal androstendione to estrone by the enzyme aromatase. Cellulite is a prototypical progressive estrogen-MMP connective tissue disorder (CTD), perpetuated by the rise and fall of menstrual hormones. The major target tissue in the uterus for both estrogen and MMPs is the endometrium, which consists mainly of collagen.
The build up and destruction of the edometrium each month during menses is a complex process orchestrated by the ebb and flow of estrogen and progesterone, which drives several different MMPs, particularly MMP 1, MMP 3, MMP 7 and MMP 9. Stromal collagen Type-1 appears to be the major target in cellulite, not the adipocytes. Prior to the appearance of ‘true cellulite,’ pendant tissue is attacked first, mainly the buttocks and the breasts. In addition to the MMP destruction, the constant gravitational force and immature biped anatomy provides no real support for these heavy structures.
Based on the aforementioned, the ‘true cellulite’ area is cited as the buttocks and thighs by scientists. Differentiation is identified by the adipocytes in this area that contain a greater number of adrenergic receptors (anti-lipolytic) than adrenergic receptors (lipolytic). These receptors account for the resistance of adipose tissue mobilization in these two anatomical sites.
The physical manifestations of cellulite are due to damage of the normal architecture of the collagen trabeculations that keep the adipose tissue confined to just two layers – the deep and the superficial layers.
What is the conclusive science connecting hormones and cellulite that we as licensed skin care professionals must understand of this condition? The answer is that cellulite is a connective tissue disorder resulting from the action of estrogen on fibroblasts to produce MMPs that damages connective tissues. This process is driven by the reproductive action causing sex hormone levels to surge. The majority of CTD in females are related to this process and scientists have been aware of the MMP action for years only recently making the critical cellulite connection.
Lifestyle, Underpants, and Cellulite
To a lesser extent, lifestyle plays a contributing role to cellulite. It has been written that the way we live is really the ultimate irritating cause of cellulite and their contributing factors that continue the controversy.
Tension, fatigue, poor eating habits, smoking, fatty and starchy foods, insufficient water intake, poor breathing, sedentary living, lack of exercise, polluted air resulting in sluggish digestion, constipation, poor circulation, standing, sitting or restriction of movement for long periods of time have all been connected to the increase of cellulite. I call it life.
It is also suspected that a high stress lifestyle is linked with cellulite because an increase of the catecholamine hormone is released into the blood stream causing imbalance of the system that ultimately activates free radical activity, exacerbating inflammation within the connective tissue.
Just when you thought it could not get any worse, it appears that our preference to what type of underwear we choose can also intensify cellulite. According to several credible references, wearing tight under garments limits blood flow to the body, triggering additional cellulite to form. Not the best news in a ‘under garment control’ fashion world. They give us a solution for hiding unsightly bulges only for us to discover these tight clothes could affect cellulite adversely. But there is a light under those tight garments; I understand there is a development in anti-cellulite panty hose to help combat the ‘cottage cheese’ that increases the blood flow to reverse the condition. I say, bring that on! The sooner the better.
Cellulite Classification
Cellulite is graded in three specific categories to determine what type of condition is present. Treatment should be rendered accordingly.
Cellulite Therapy
Now that we have a comprehensive understanding of the cause and effect of cellulite, we must turn to the immediate and long-term solutions to manage this condition. Numerous therapies have been developed and initiated to control cellulite. Unfortunately, with the buffet of different remedies available via retail, professional, and medical means, there are no published reports in the scientific literature substantiating that any of these modalities work to rid the condition. Manage cellulite, yes; eradicate cellulite, no. Having established this fact, it is the responsibility of the licensed aesthetic professional to provide a ‘management system’ for a cellulite condition and do further research on the many modalities available to ensure the remedy you select is compatible for the condition and grade of the cellulite to be treated. Keep in mind; it will require more than one remedy to achieve management success.
Some of the more popular physical, mechanical, and product methods to treat cellulite are: Iontophoresis; ultrasound; thermotherapy; pressotherapy (pneumatic massaging in the direction of the circulation); lymphatic drainage (gentle massage to stimulate lymphatic flow and reduce tissue inflammation); electrolipophoresis (application of a low frequency electric current); creams and gels that contain pharmaceutical and cosmetic agents such as mexthyxanthines (theobromine, theophylline, aminophylline, caffeine) which act through phosphodiesterase inhibition, and pentoxifylline that improves microcirculation; the adrenergic beta-agonists isoproterenol and adrenaline; the adrenergic alpha-antagonists yohimbine, piperoxan, phentolamine, and dihydroergotamine; the methylxanthine enhancers Coenzyme A and the amino acid l-carnitine; the drugs with connective tissue activity sillicium and Asiatic centella; and the microcirculation active drugs Indian chestnut, gingko biloba, and rutin in different combinations and application methods.
Given all the expensive and experimental treatment options via aesthetic mechanical and medical means, there still remains an alternative choice with the application of daily cellulite creams and lotions. Many formulas have a solid history in achieving results because these products are used daily and have been developed to target cellulite. These formulas produce temporary results, therefore must be used every day to be effective in controlling cellulite. Specialized cellulite creams and lotions can have a significant and dramatic effect when directions are followed specifically. Adipose tissue can be reduced with specific lypolytic agents and the best products contain ingredients to target the cellulite tissue to help reverse the ‘orange peel’ condition.
In conclusion, cellulite is never cured, only supervised with a careful selection of treatment. This ‘dimple disease’ requires a continued healthy diet, exercise, massage, and proven products by which this genetically predisposed, hormone driven fat condition is controlled and managed for effective endpoint results.
An inducted Legend in American Aesthetics by DERMASCOPE Magazine and Aesthetics International Association (AIA) in 2008, Christine Heathman has been a practicing licensed master aesthetician, educator, and a leader in the research and development of skin care and progressive clinical protocols for over 25 years. A recent testimonial to Heathman’s skin knowledge selected her amazing product formulas out of thousands and recently featured them on the nationally syndicated TV show called The Doctors, as an alternative option to cosmetic surgery. www.glymedplus.com
Sclerotherapy of Varicose Veins with Polidocanol Based on the Guidelines of the German Society of Phlebology
Abstract
BACKGROUND Sclerotherapy involves the injection of a sclerosing agent for the elimination of intracutaneous, subcutaneous, and transfascial varicose veins.
OBJECTIVE To update guidelines for sclerotherapy of varicose veins.
METHODS The guidelines for sclerotherapy of varicose veins of the German Society of Phlebology were updated and modified through a review of the available literature.
RESULTS Published clinical series and controlled clinical trials provide evidence to support the elimination of intracutaneous and subcutaneous varicose veins using sclerotherapy. Allergic skin reactions occur occasionally as allergic dermatitis, contact urticaria, or erythema. Anaphylaxis is rare. Transient migraine headaches present more frequently in patients treated with foam sclerotherapy than liquid sclerotherapy.
CONCLUSION Sclerotherapy is the method of choice for the treatment of small‐caliber varicose veins (reticular varicose veins, spider veins). If performed properly, sclerotherapy is an efficient treatment method with a low incidence of complications.
BioForm Medical provided financial support for formal formatting of this manuscript without any influence over the content of the manuscript. The authors have previously participated in two scientific studies with polidocanol (ESAF and EASI study) financed by Kreussler.
Sclerotherapy involves the injection of a sclerosing agent for the targeted elimination of intracutaneous, subcutaneous, and transfascial varicose veins (perforating veins) and the sclerosation of subfascial veins in the case of venous malformation. Various sclerosants induce marked damage of the vascular endothelium and possibly of the entire vascular wall. After successful sclerotherapy and in the long term, the veins are transformed into a fibrous cord, a process known as sclerosis.1, 2 The purpose of sclerotherapy is not merely to achieve thrombosis of the vessel, which per se may be amenable to recanalization, but definitive transformation into a fibrous cord. This cord cannot recanalize, and the functional result is equivalent to the surgical removal of a varicose vein.
Indications
The guidelines for sclerotherapy of varicose veins of the German Society of Phlebology were slightly modified and updated with the results from recently published data.3
The objectives of sclerotherapy are:
- •Treatment of varicose veins and prevention of possible complications.
- •Reduction or elimination of existing symptoms.
- •Improvement of pathologically altered venoushemodynamics.
- •Achievement of good results that satisfy aesthetic and functional criteria.
In principle, all types of varicose veins are amenable to sclerotherapy. Particular indications are listed in Table 1.
| • Saphenous veins (great saphenous vein and small saphenous vein) |
| • Accessory saphenous veins |
| • Varicose veins associated with perforator incompetence |
| • Reticular veins |
| • Telangiectases |
| • Residual and recurrent varicose veins after treatment |
| • Pudendal and genital varicose veins |
| • Peri‐ulcerous veins |
| • Venous malformations |
Sclerotherapy is the method of choice for the treatment of small‐caliber varicose veins (reticular varicose veins, spider veins). For the obliteration of accessory varicose veins and incompetent perforating veins, sclerotherapy competes with percutaneous phlebectomy and with ligation of perforating veins or endoscopic dissection of perforating veins.4, 5 In the treatment of saphenous veins, surgery has been the method of choice, but treatment of truncal veins using sclerotherapy is also possible.6–8 This applies in particular to foam sclerotherapy, as studies conducted in recent years have demonstrated.9–13
Contraindications
Absolute and relative contraindications are listed in Table 2.
| Absolute contraindications |
Relative contraindications |
|---|---|
| Liquid and foam sclerotherapy: • Known allergy to the sclerosant • Severe systemic disease • Acute deep vein thrombosis • Local infection in the area of sclerotherapy or severe generalized infection • Lasting immobility and confinement to bed • Advanced peripheral arterial occlusive disease (Stage III or IV) • Pregnancy (unless a compelling medical reason exists) Foam sclerotherapy: • Known symptomatic patent foramen ovale |
Liquid and foam sclerotherapy: • Leg edema, uncompensated • Late complications of diabetes (e.g., polyneuropathy) • Arterial occlusive disease, Stage II • Poor general health • Bronchial asthma • Marked allergic diathesis • Known thrombophilia or hypercoagulable state with or without a history of deep vein thrombosis Foam sclerotherapy: • Known asymptomatic patent foramen ovale • High risk of thromboembolic events • Visual disturbances or neurological disturbances after previous foam sclerotherapy |
Complications and Risks
If performed properly, sclerotherapy is an efficient treatment method with a low incidence of complications. In therapy, a number of adverse events may be encountered. These are shown in Table 3.14–17
| • Allergic reaction |
| • Skin necroses |
| • Excessive sclerosing reaction |
| • Pigmentation |
| • Matting |
| • Nerve damage |
| • Scintillating scotomas |
| • Migraine‐like symptoms |
| • Orthostatic collapse |
| • Thromboembolism |
Allergic skin reactions occur occasionally as allergic dermatitis, contact urticaria, or erythema. Anaphylactic shock and inadvertent intra‐arterial injection are extremely rare complications constituting an emergency situation.18, 19 Transient migraine‐like symptoms occur more commonly after foam sclerotherapy than after liquid sclerotherapy.14, 17 In this context, it has been speculated that a patent foramen ovale (PFO), which is present in approximately 25% of the population, might be a factor, allowing foam bubbles to pass into the arterial circulation.18–22
Thromboembolic events [deep vein thrombosis (DVT), pulmonary embolism or stroke] occur in rare circumstances after sclerotherapy. Most of these events, diagnosed in routinely performed duplex investigations, are asymptomatic.14, 17 According to prospective studies, the risk of DVT is higher when larger volumes of sclerosant are used, particularly in the form of foam9, 23–25 and in patients with a previous history of thromboembolism or known thrombophilia.26 In patients with these risk factors, the indication for sclerotherapy must be clearly established, and additional precautionary measures must be observed.27 Single case reports of proven stroke or transient ischemic attack after liquid or foam sclerotherapy in patients with PFO have been published.17, 23, 28, 29 Multiple small‐dose injections of foam can reduce the passage of sclerosant foam into deep veins.30
Skin necroses have been described after perivascular injection of sclerosants in higher concentrations and rarely after properly performed intravascular injection with sclerosants in various concentrations, for example, with 0.5% polidocanol in the treatment of spider veins.31In the latter case, a mechanism involving passage of the sclerosant into the arterial circulation via arteriovenous anastomoses has been suggested.32 In individual cases, this has been described as embolia cutis medicamentosa.33 Extensive necroses occur after inadvertent intra‐arterial injection.31, 34 Instances of hyperpigmentation have been reported, with frequencies ranging from 0.3% to 10%.15, 35 In general, this phenomenon regresses slowly. The incidence of pigmentation is likely to be higher after foam sclerotherapy.14 Matting¯ in the area of a sclerosed vein¯ is an unpredictable individual reaction of the patient and can also occur after surgical removal of a varicose vein.31 Local paresthesia after sclerotherapy is rare.36, 37
Other transitory phenomena after sclerotherapy include intravascular clots, phlebitis, hematomas, disturbed sense of taste, feeling of tightness in the chest, pain at the injection site, swelling, induration, mild cardiovascular reactions, and nausea. Additionally, complications such as blister formation (blisters in the vicinity of an adhesive plaster) may arise because of the compressive bandage.4 Intravascular clots can be squeezed out after a stab incision to reduce the development of hyperpigmentation.
Diagnosis Before Sclerotherapy
To be successful, sclerotherapy requires thorough planning. Therefore, a proper diagnostic evaluation should be performed before treatment.3 Diagnostic evaluation includes history‐taking, clinical examination, and Doppler ultrasound investigation. Functional examinations make it possible to assess improvement in venous function, which is to be expected for the elimination of varicosis. Diagnostic imaging is especially suitable for identifying incompetent junctions with the deep venous system and for locating pathologic reflux, as well as for clarifying post‐thrombotic changes and selecting the most appropriate treatment option. In addition, sclerotherapy is an intervention that requires patients’ informed consent.
Implementation of Sclerotherapy of Varicose Veins Using Polidocanol
Polidocanol in concentrations of 0.25%, 0.5%, 1%, 2%, 3%, and 4% is licensed in Germany for sclerotherapy of varicose veins. The maximum daily dose of polidocanol is 2 mg/kg of body weight.38
Sclerotherapy with Sclerosing Solutions (Liquid Sclerotherapy)
Table 4 provides guide values for concentration and volume per injection for liquid sclerotherapy.38
| Indications | Volume Per Injection, mL | Concentration % |
|---|---|---|
| Spider veins | 0.1–0.2 | 0.25–0.5 |
| Central veins of spider veins | 0.1–0.2 | 0.25–1 |
| Reticular varicose veins | 0.1–0.3 | 1 |
| Small varicose veins | 0.1–0.3 | 1 |
| Medium‐size varicose veins | 0.5–2.0 | 2–3 |
| Large varicose veins | 1.0–2.0 | 3–4 |
A smoothly functioning disposable or glass syringe and a small‐diameter cannula are required for sclerotherapy. Cotton‐wool rolls or pads and adhesive paper tapes are used for local compression. The different techniques vary considerably. The following principles apply to liquid sclerotherapy:
- •Puncture of the veins can be performed with the patient standing or lying down.
- •The injection is usually performed with the patient in a supine position. After the vein has been punctured with the free injection needle or with the syringe attached, the intravascular position is checked.
- •Intravascular injection of the sclerosant is performed slowly and incrementally, checking that the cannula is positioned inside the vein. Severe pain during injection may be indicative of perivascular injection.
- •Immediately after injection of the sclerosant and removal of the cannula, local compression is performed along the course of the sclerosed vein.
- •After sclerotherapy, compression is applied to the treated extremity. Compression can be performed using a compression stocking and a compression bandage.
- •Local compression can be removed the same evening or the next day. Depending on the diameter and location of the varicose veins, compression is performed for hours up to several days and weeks after completion of sclerotherapy.
- •After a sclerotherapy session using the traditional technique, the patient should ambulate (physical thromboprophylaxis). Careful watch must be kept for any signs of allergic reactions.
- •Intensive sports activity, hot baths, sauna, and strong ultraviolet irradiation (solarium use) should be avoided in the initial days after sclerotherapy.
Sclerotherapy with Foamed Sclerosants (Foam Sclerotherapy)
The literature has long contained reports of sclerotherapy with foamed sclerosants.39 In recent years, as the technology has improved, foam sclerotherapy has become established, particularly for the treatment of larger varicose veins.40, 41 Detergent‐type sclerosants such as polidocanol can be transformed into fine‐bubbled foam using special techniques.
In the Monfreux technique,41 negative pressure is generated by drawing back the plunger of a glass syringe, the tip of which is tightly closed. The resulting influx of air produces large‐bubbled, fairly fluid foam.39 In the Tessari technique, the turbulent mixture of liquid and air in two syringes connected using a three‐way stopcock produces the foam. It is fine‐bubbled and fluid at low concentrations and rather viscous at high concentrations. The mixing ratio for sclerosant to air is 1:3 to 1:4. The double syringe system technique involves the turbulent mixing of polidocanol with air in a sclerosant to air ratio of 1:4 in two syringes linked using a connector. The resulting product is fine‐bubbled, viscous foam.39
The standardized transformation of a licensed liquid sclerosant into a foam sclerosant and treatment with it is permissible provided that the patient has been adequately informed about the procedure and about the benefits and risks of the method and consents to its use. Even if foam is used off‐label, the published evidence and data document the use as a standard procedure.
The Second European Consensus Conference on Foam Sclerotherapy took place at Tegernsee, Germany in April 2006. On the basis of the expert’s own experience and the available literature, the following recommendations on foam sclerotherapy were given, partially modified for the guideline.27
Puncture and Injection
When treating the great saphenous vein (GSV) by direct puncture, it is recommended that venous puncture be performed in the proximal thigh area. If long catheters are used, it is recommended that access to the GSV be made below the knee. When treating the short saphenous vein (SSV) by direct puncture, it is recommended that venous puncture be performed in the proximal or middle part of the lower leg. When treating the perforating veins, it is recommended that the injection not be made directly into the affected vein.
Foam Generation, Concentrations, and Volumes
The Tessari and Tessari/double syringe system methods are recommended for the generation of foam sclerosant for all indications. Air is accepted or proposed as the gas component for the generation of foam sclerosant for all indications. A mixture of carbon dioxide and oxygen may also be used. The preferred ratio of liquid sclerosant and gas for the generation of a foam sclerosant is 1:4 (1 part liquid to 4 parts gas). Ratios between 1:1 and 1:5 are used for reticular varicose veins and spider veins, but the majority use the 1:4 ratio. The preferred foam volumes per venous puncture are shown in Table 5, and the preferred concentrations are outlined in Table 6. The recommended maximum foam volume per leg and session (given in a single injection or in several injections) is 10 mL. When treating large‐caliber varicose veins, the foam sclerosant should be as viscous as possible.
| Mean Foam Volume Per Puncture, mL |
Maximum Foam Volume Per Puncture, mL |
|
|---|---|---|
| GSV | 2–4 | 6 |
| SSV | 2–4 | 4 |
| Collateral veins | Up to 4 | 6 |
| Recurrent varicose veins | Up to 4 | 8 |
| Perforating veins | Up to 2 | 4 |
| Reticular varicose veins | <0.5 | <1 |
| Spider veins | <0.5 | <0.5 |
| Venous malformations | 2–6 | <8 |
| Liquid | 0.25% | 0.5% | 1% | 2% | 3% | 4% | |
|---|---|---|---|---|---|---|---|
| Great saphenous vein | + | ++ | ++ | ||||
| Small saphenous vein | + | ++ | + | ||||
| Collateral veins | ++ | ||||||
| Recurrent varicose veins | (+) | ++ | ++ | + | |||
| Perforating veins | (+) | ++ | + | (+) | |||
| Reticular varicose veins | (+) | (+) | ++ | + | |||
| Spider veins* | ++ | (+) | (+) | ||||
| Venous malformations | + | ++ | + |
- The stated concentrations refer to the liquid polidocanol solution from which foam is generated.
- * Foam sclerotherapy is not the treatment of choice for vessels smaller than 1 mm in diameter. For sclerotherapy of spider veins the recommendation is first to use liquid polidocanol. When foam is used, small volumes of 0.25% foam are preferred.
Safety Measures
Safety during foam sclerotherapy of the GSV and SSV can be improved by avoiding immediate compression of the injected areas, using ultrasound to monitor foam distribution, injecting a highly viscous foam, and ensuring that there is no patient or leg movement for 5 minutes and no Valsalva maneuver or other muscle movement.
The known presence of a PFO indicates that sclerotherapy must be performed with special precaution. Such patients patient should remain lying down for longer (8 to 30 minutes), use only small volumes of foam (2 mL) or liquid sclerotherapy, and avoid Valsalva maneuvers.
Before foam sclerotherapy, it is not considered necessary to perform specific investigations for PFO.
A high risk of thromboembolism in the patient’s history and known thrombophilia (especially in combination with a high risk of thromboembolism) indicates that sclerotherapy must be performed with special precaution. It is recommended that, in such patients, adequate low‐molecular‐weight heparin prophylaxis (in line with relevant guidelines and recommendations) be instituted, physical prophylaxis be implemented, low sclerosant concentrations be used for foam generation, and small volumes of foam be used. The practitioner is advised to perform a benefit‐risk assessment based on the particular indication.
It is not considered necessary to perform specific investigations for thrombophilia before foam sclerotherapy.
Patient Information
Before foam sclerotherapy, patients should be informed about risks and possible adverse effects in the same way as before liquid sclerotherapy. In addition, they should be told that there is a slightly higher risk of hyperpigmentation and inflammation, there is a risk of developing (transient) neurological symptoms, there is a risk of developing (transient) visual disturbances, and there is a risk of triggering migraine.
As before liquid sclerotherapy, patients should be informed about the expected treatment outcome. In addition, they should be told that short‐term outcomes are highly satisfactory; further therapy is possible and may be necessary in some cases, especially in treatment of large varicose veins; and foam sclerotherapy is more effective than liquid sclerotherapy.
Efficacy
Numerous published clinical series and controlled clinical trials provide evidence to corroborate the elimination of intracutaneous and subcutaneous varicose veins using sclerotherapy.
In older studies with liquid sclerotherapy, surgery was significantly more effective in the treatment of saphenous varices.4 In the treatment of saphenous varicose veins, foam sclerotherapy is significantly more effective than liquid sclerotherapy.11, 13, 42–44 The immediate occlusion rate of the GSV after foam sclerotherapy reaches 70% to 95%.9–13 After 1 to 3 years of follow‐up, the occlusion rate drops to 55% to 80%.9, 11, 12, 45, 46 The occlusion rate depends on the initial diameter of the vein and the injected foam volume and concentration.13, 25 Long catheter‐assisted foam sclerotherapy of the GSV, with or without terminal balloon, seems to have slightly better occlusion rates.47–51 Foam sclerotherapy is also more effective in the treatment of venous malformations than liquid sclerotherapy.43 In the treatment of accessory varicose veins, liquid sclerotherapy is less effective than surgery.52In contrast, occlusion rates after foam sclerotherapy are better than those in saphenous veins.53 The occlusion rate after 3 years reaches 80%.53 In patients with venous ulcers, sclerotherapy of peri‐ulcer varices improves ulcer healing.54–56 Sclerotherapy is the standard treatment for intracutaneous varicose veins (telangiectases and reticular veins), allowing improvement of up to 90% to be achieved.57–60
Compression treatment with medical compression stockings may improve the results of sclerotherapy for spider veins.35, 61 The incidence of pigmentation decreases significantly.35, 62 Local eccentric compression significantly increases local pressure in the sclerosed area and improves the efficacy of sclerotherapy.63
Where Practices Waste Money Venus Concepts
Many medical aesthetics clinics face financial challenges and don’t have an adequate grasp on their numbers. It’s understandable—it can be difficult to determine the return on investment (ROI) of individual expenses, especially the ones that aren’t directly connected to profits. Getting an idea of the areas in which aesthetics clinics like yours are bleeding money can help to better determine what’s worth your investment and where it may be more appropriate to cut corners or expenses altogether. Get a better understanding of your financials and identify cost-saving initiatives for your clinic by considering the following areas where medical aesthetics clinics and MediSpas often waste the most money.
Top Money-Wasters for Medical Aesthetics Clinics
Print Advertisements
There is a place and time for printed advertising but oftentimes, they can be a waste of money and resources. When introducing a new device or treatment to your clinic, for example, posters in your waiting room and a few brochures for those who prefer print may be beneficial in catching some attention from current patients. However, in many cases, digital marketing materials can offer a greater value.
Informative and downloadable marketing packages can be hosted on your website to which you can link via social media posts or email advertisements, making it possible to use one versatile piece on multiple platforms. As well, the use of these digital communications can be better targeted to interested parties while saving on material costs for paper and printing, thereby lowering marketing costs and boosting your ROI. Digital files also take up much less storage space, making this a money-saver in a variety of ways. Finally, digital communications offer a longer lifespan as details can easily be updated without having to toss anything out. If print assets are still a necessary requirement for your patient base—perhaps if a large chunk of your patient base is much older—then look for device companies that offer patient brochures, posters, and other marketing collateral for purchase. This would enable you to still provide print advertising for your patients without incurring the additional costs of designing or printing.
Inefficient Processes
Everyday processes can be significant time-wasters. While calling patients to remind them of upcoming appointments can help prevent last-minute cancellations, this process can also take up a lot of your staff’s time, and their time costs you a decent amount of money. Instead, consider introducing new applications that automatically send reminders via email or text message. Offering online bookings can also help to better manage appointments for patients who don’t require questions to be answered prior to their consultation or treatment sessions. To determine the inefficiencies costing your clinic the most in time and money, consider sitting down with each of your staff and asking them about their most time-consuming tasks or areas where they see redundancies that could be resolved simply by introducing new software, applications, or processes.
Buying the Same Old Supplies
It can be easy to fall into simple habits, like purchasing table paper, cleaning supplies, syringes, and more from the same old supplier. While establishing a long-running supplier can sometimes lock your clinic in at lower prices for these everyday consumables, it could also mean that you’re overpaying for the same old supplies. Becoming comfortable in your purchasing habits could leave you missing out on deals and new competitive pricing. Instead of falling into a routine, consider taking a close look at supply costs on an annual basis. Look at separate items to see if there is anything that seems to be a little too costly or if you could perhaps buy in a larger quantity to save on your per-unit costs. If competitors reach out to your clinic with attractive pricing offers, take the time to listen to their proposals, ask questions, and consider making the switch. Cutting these costs altogether is often out of the question; your clinic simply can’t function without these supplies after all. However, you can save on their costs, so don’t let this money-waster slip by without review.
Bad Hires and Unhappy Staff
Rushing the hiring process or neglecting to keep staff happy not only leads to wasted money on staffing costs when they inevitably quit, but it can also be a drag on your clinic’s patient satisfaction and retention ratings. While extending the hiring period for new staff may be a little more costly and potentially risk having a position remain open for a period, it’s not worth the risk hiring a candidate who isn’t the perfect fit for both the position and your staff. Investing in career development and continuing education for employees, and scheduling regular meetings with each staff member to review their roles, concerns, and goals can keep everyone feeling challenged and a part of the team, leading to improved employee and patient satisfaction.
Too Many Marketing Strategies
It might be tempting to try every marketing strategy out of fear you may miss gathering the attention of some prospective patients. However, the broader your marketing strategy, the more costly and less effective it becomes. Efforts between print and digital platforms are spread too thinly and marketing dollars don’t match up to your ROI. Instead of doing it all, focus in on two or three marketing strategies that best target your ideal prospective patient and show adequate returns based on your marketing goals. In other words, aim for a marketing make-under to improve patient acquisition and get the most out of your marketing dollars.
Office Space
Office space accounts for about eight to 15% of revenue for most clinics. Based on this alone, leaving treatment rooms unused or having a large waiting room space that is never filled could be costing your clinic a lot of money. Get creative with the square footage you’re paying for and ensure you’re getting the most out of your space. If your clinic is efficient enough or has an adequate number of treatment rooms that your waiting room is rarely in use, consider renovating to convert a portion of it into a new, more useful space based on your clinic’s needs. Alternatively, if you have an extra treatment room that’s rarely used, consider converting it into a dedicated photography space for better before-and-after pictures you can use to strengthen your marketing efforts. You may also consider renting often unused space to an aesthetician or dermatologist with dedicated hours to not only bring in more patients, but also convert what used to be a money-wasting cost into a money-making strategy.
Not Reading the Fine Print
Skipping out on your due diligence when signing contracts for services, equipment, rental space, and more can lead to a hefty amount of lost money. Before signing on the dotted line, review all the details of your contract and ensure it matches what you agreed upon in your negotiations. If anything is unclear, ask for clarification and confirm that you understand every last clause before adding your signature. Note that sales representatives and vendors can leave or change over time, so any verbal agreements won’t stand. Get everything in writing, have it signed, and push for price protection should the status quo change.
Fluctuating Costs
Keeping track of all your clinic’s finances can seem daunting, but it’s necessary to ensure your clinic is running efficiently, treatments are properly priced, and promotions aren’t undercutting your bottom line. Don’t make the excuse that you don’t have enough time to consider your financials regularly. Instead, work towards spotting areas in which you can swap out fluctuating costs with consistent monthly charges. By focusing in on predictable expenses, identifying or estimating your clinic’s average monthly expenses becomes much easier, allowing you to better calculate your ROIs and reallocate money from areas that aren’t paying off to business strategies that could use a bigger investment for a better return.
To begin, consider a Venus Concept partnership. With each device purchase, your clinic gains access to ongoing clinical education for your staff, professionally designed print and digital marketing assets, practice consulting and marketing support, industry-leading technology, comprehensive warranty coverage, and easy device upgrades all through the industry’s first and only true subscription acquisition model. To learn more about the cost-saving benefits of a Venus Concept partnership, contact an expert today!

